Pathophysiology and Development
Pathophysiology and Development
PD is a progressive, chronic, neurodegenerative disease characterized by slow and selective loss of dopaminergic neurons, with accumulation of Lewy bodies in the substantia nigra. It is generally responsive to levodopa or dopaminergic treatment, which are the foundations of management.
Motor signs of PD are thought to result in large part from dopamine impairment in the basal ganglia and related areas in the thalamus and cortex. Evidence has implicated electrophysiologic changes (altered discharge rates, increased incidence of burst firing, interneuronal synchrony, oscillatory activity, and altered sensorimotor processing) in PD, which underscores the disease as a complex network disorder. Abnormal activity in groups of neurons in the basal ganglia strongly affect excitability, oscillatory activity, synchrony and sensory responses in the cerebral cortex, thereby impairing the planning and execution of movement, along with executive, limbic and/or sensory functions.
PD consists of a premotor/prodromal period that can begin years to decades before motor symptoms present and diagnosis is established. (Figure 1)
Figure 1: Time Course of PD Progression
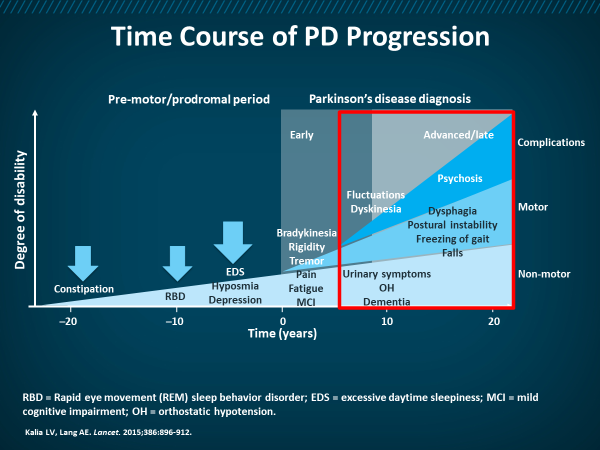
Cardinal motor features of PD include bradykinesia, rest tremor, and rigidity, which generally appear early in the disease course and largely depend on dopaminergic nigrostriatal denervation. Intermediate and advanced PD stages are generally ruled by motor fluctuations and dyskinesia, which are linked to complex mechanisms related to nigrostriatal loss and inhibition of levodopa absorption.
Other features of PD can include nondopaminergic dysfunction resulting in motor problems, such as posture, balance and gait disturbances, and fatigue, and nonmotor problems that may include depression, apathy, cognitive impairment, sleep disturbances, pain, autonomic dysfunction, and others.
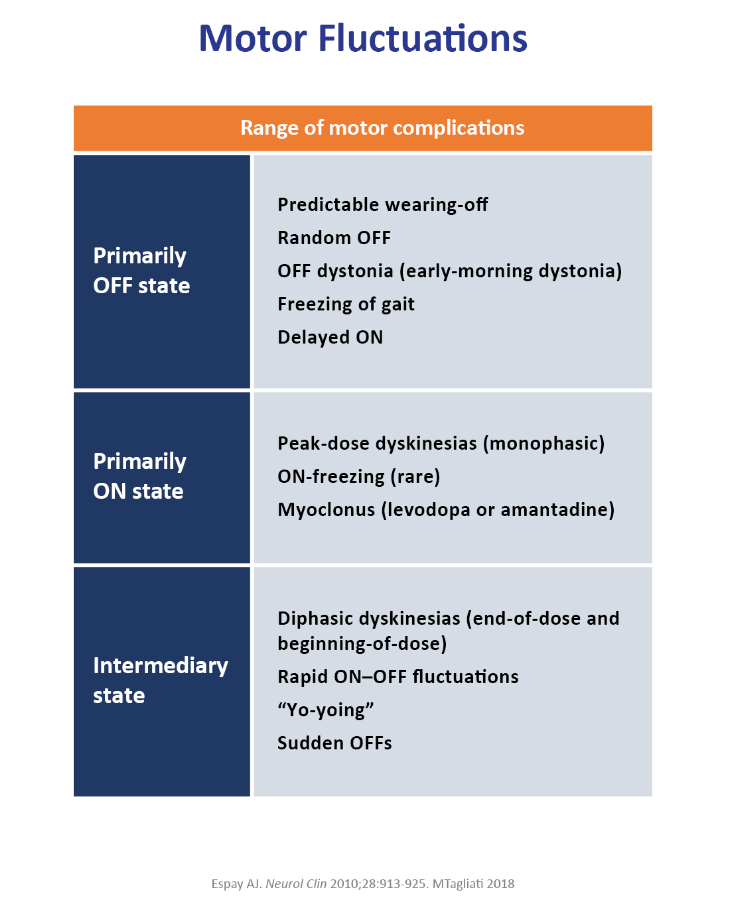
Motor fluctuations vary widely in PD, with on, off, and intermediary states. (Figure 2) The off state is characterized by predictable wearing off, freezing of gait, early-morning dystonia and others, while the on state can involve peak-dose dyskinesias, on-freezing and others. The intermediary state can involve rapid on/off fluctuations and yo-yoing between the two states.
Figure 2: Motor Fluctuations in PD
Evolving understanding of neuropathological, neurochemical, and neurophysiological bases of PD and its motor/nonmotor symptoms offer the rationale for current therapeutic approaches of this condition and also represent a foundation for studying future avenues of research.
References
Espay AJ. Management of motor complications in Parkinson disease: current and emerging therapies. Neurol Clin. 2010;28:913-925.
Galvan A, Wichmann T. Pathophysiology of Parkinsonism. Clin Neurophysiol. 2008;119(7):1459–1474.
Kalia LV, Lang AE. Parkinson’s Disease. Lancet. 2015;386:896-912.
Magrinelli F, et al. Pathophysiology of Motor Dysfunction in Parkinson’s Disease as the Rationale for Drug Treatment and Rehabilitation. Parkinsons Dis. 2016;2016:9832839.