Managing OFF Episodes
As Parkinson’s disease (PD) progresses, patients begin to experience increasingly frequent periods of poor symptom control known as OFF episodes. These fluctuations in symptom control become more prevalent over time, with approximately 10% of patients developing motor fluctuations each year after the onset of levodopa initiation.1,2 After 4 to 6 years, 40% of patients with PD report motor fluctuations, and nearly all patients experience them after 10 years.
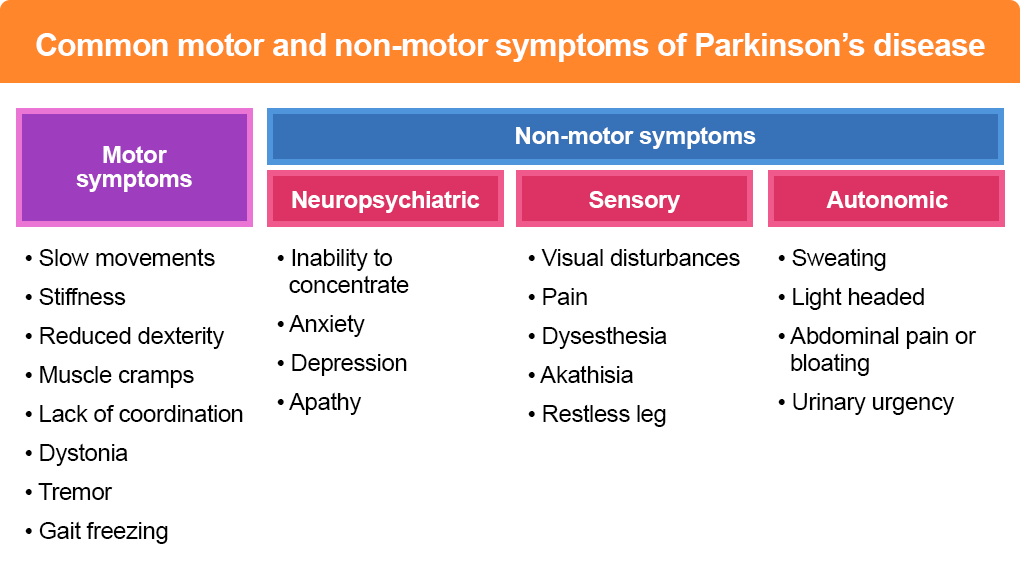
The motor symptoms experienced by patients in the OFF state are variable. Some patients report a mixture of slow movements, stiffness, reduced dexterity, muscle cramping, and lack of coordination. Others experience difficulties in their ability to stand up, balance, or even swallow. Patients may suffer from changes in their voice or breathing while experiencing dystonia in their hands, feet, or legs. Occasionally, worsening of tremor and the emergence of gait freezing can be seen.3
Non-motor symptoms may also occur during OFF episodes. Neuropsychiatric symptoms may present as fluctuations in cognition or attention, or anxiety, depression, and apathy. Patients with PD may also experience autonomic symptoms such as altered sweating, light-headedness, abdominal pain or bloating, or urinary urgency. Sensory symptoms sometimes reported include visual disturbances, pain, dysesthesia, akathisia, and restless leg. Motor and non-motor fluctuations are a major source of disability and lead to a substantially reduced quality of life.4,5
Figure 1: Common motor and non-motor symptoms of Parkinson’s disease4,5
There are several broad categories of OFF episodes that can impact a patient with PD. An “early morning” OFF state is the occurrence of slowness or immobility in a patient’s waking hours prior to the first medication dose of the day. This is related to low plasma levodopa levels from a lack of medication overnight.6
“Wearing off” refers to the gradual transitions in symptom control toward the end of a medication dose. These “wearing off” episodes may be caused by changes to levodopa half-life, issues with presynaptic storage, or dopamine receptor internalization.6 “Delayed on” describes the lengthy latency for a levodopa dose to start working and can commonly occur with the first morning dose or after a meal.
“Dose failure” occurs when the medication fails to work and no “ON time” occurs after a medication dose. “Delayed on” and “dose failure” episodes may be caused by gastric emptying delays, abnormal intestinal absorption, or delays in transport across the blood brain barrier.6 “Unpredictable OFF” episodes may also occur suddenly with the development of OFF symptoms within seconds or minutes.
Figure 2: Schematic representation of OFF episodes in Parkinson’s disease6
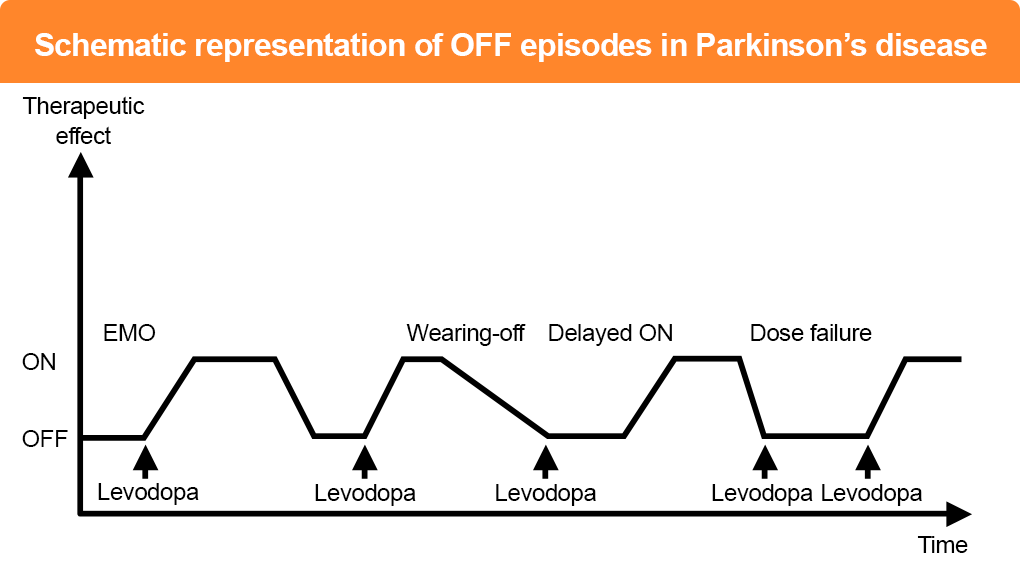
EMO = early morning OFF
One strategy to reduce motor fluctuations is to increase levodopa concentrations and duration of activity through the use of adjunctive medications, which can be achieved by interfering with dopamine and levodopa metabolism or by using dopamine agonists that mimic the action of dopamine.6
Levodopa is metabolized peripherally by the enzyme catechol-O-methyl transferase (COMT). Drugs that inhibit COMT increase the bioavailability and elimination half-life of levodopa, thereby decreasing OFF episodes through sustained dopaminergic stimulation.6 Other drugs inhibit monoamine oxidase-B, an enzyme that degrades dopamine in the synaptic cleft.6
In PD, higher doses of levodopa are associated with increased risk of motor and non-motor complications. Dopamine agonists reduce OFF time by directly stimulating striatal postsynaptic receptors and can be valuable to patients with motor complications as they improve OFF times without increasing levodopa.6 Despite optimal use of oral dopaminergic therapy, patients with PD can suffer up to 2 to 3 hours of OFF time per day on average.
On-demand, rapid-acting medications can provide quick symptom control during dose failures and unpredictable OFF periods.6 A levodopa inhaler is also available for the intermittent treatment of OFF episodes and allows for rapid absorption with clinical effects noted as soon as 10 minutes after administration.7,8 Levodopa/carbidopa may also be administered enterally via a percutaneous endoscopic gastrostomy with jejunal extension (PEG-J) or nasojejunal tube.
Apomorphine is a potent dopamine agonist with a broad spectrum of effects on both D1- and D2-like receptors. After a subcutaneous injection via a multidose pen, peak blood concentration is reached within 10 minutes and a maximum cerebrospinal fluid concentration is achieved within 30 minutes. However, some patients with PD struggle to administer a pen injection during an acute OFF phase, and less invasive delivery systems are available.6 Sublingual apomorphine has comparable symptomatic effects to subcutaneous administration and is indicated for the acute, intermittent treatment of OFF episodes. In clinical trials, sublingual apomorphine achieved an “ON” state within 15 to 30 minutes of administration for the majority of patients with PD.
References
- Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesia and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001;16:448-458.
- Katzenschlager R, Head J, Schrag A, et al. Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology. 2008;71:474-480.
- Stacy M. The wearing-off phenomenon and the use of questionnaires to facilitate its recognition in Parkinson’s disease. J Neural Transm (Vienna). 2010;117:837-846.
- Chaudhuri KR, Prieto-Jurcynska C, Naidu Y, et al. The nondeclaration of nonmotor symptoms of Parkinson’s disease to health care professionals: An international study using the nonmotor symptoms questionnaire. Mov Disord. 2010;25:704-709.
- Martínez-Fernández R, Schmitt E, Martinez-Martin P, Krack P. The hidden sister of motor fluctuations in Parkinson’s disease: A review on nonmotor fluctuations. Mov Disord. 2016;31:1080-1094.
- Vijiaratnam N, Foltynie T. Therapeutic strategies to treat or prevent off episodes in adults with Parkinson’s disease. Drugs. 2020;80:775-796.
- Olanow CW, Factor SA, Espay AJ, et al. Apomorphine sublingual film for off episodes in Parkinson’s disease: A randomised, double-blind, placebo-controlled phase 3 study. Lancet Neurol. 2020;19:135-144.
- Paik J. Levodopa inhalation powder: A review in Parkinson’s disease. Drugs. 2020;80:821-828.